Pain, stiffness and swelling: Osteoarthritis affects women twice as much as men
By Grace McGettigan
31st Mar 2021
31st Mar 2021
World Arthritis Day osteoarthritis
Osteoarthritis is on the rise in Ireland, and as it affects twice as many women as men, we’re shedding a light on the condition. We spoke with Dr Helen French, a senior lecturer in physiotherapy at RCSI and clinical specialist physiotherapist, to learn more.
Pain when moving? Reduced flexibility and stiff joints that are tender to the touch? These are just some of the symptoms of osteoarthritis; a condition affecting twice as many women as men. What’s more, diagnoses of the condition are on the rise in Ireland.
One in five women are at risk of developing the disease – but with the right knowledge and careful management, there’s no reason why people with osteoarthritis can’t live a relatively healthy life.
We spoke with Dr Helen French, a senior lecturer in physiotherapy at RCSI and clinical specialist physiotherapist, about what osteoarthritis is, how it can impact our quality of life, as well as how to best prevent it.
What is osteoarthritis?
Arthritis is a condition of the joints – such as our elbow, shoulder or knee – and impacts our ability to move. There are various types of it, with osteoarthritis being the most common.
“Osteoarthritis affects the cartilage of the joint,” says Dr French. “The cartilage is like a shock absorber. It’s a little bit softer than bone, but it allows that ‘cushion’ and shock absorption.
“People often think it’s a normal part of ageing, which is incorrect.”
“With osteoarthritis, the most common joints affected are the knees, then the hips, and then the hands,” she says. While some people have the disease in just one joint, Dr French says it’s more common to have it in a few joints, such as both knees and hips, or one knee and both hands.
It’s important to note that osteoarthritis is not a normal part of growing old. “People often think it’s a normal part of ageing, which is incorrect,” says Dr French. “People often say, ‘Oh, it’s just old age that I’ve got these pains in my joints,” and that’s a myth we want to dispel because, if they think it’s normal, then they kind of put up with it and don’t seek help.”
Impact on day-to-day life
Symptoms of osteoarthritis often develop slowly, and if not well-managed, they can worsen over time. These symptoms include pain when moving, a loss of flexibility and/or stiffness in the joint, as well as tenderness to the touch. Other symptoms can include swelling around the joint, as well as a grating or ‘popping’ sound when you move.
“The main symptom that people will start to notice is pain,” says Dr French. “Pain will be the reason why somebody actually says ‘I need to go and get help here’.”
What’s more, this pain tends to get worse over time. “If we take a hip or knee, it might start off with pain with running, but then it can progress to pain with walking. It can be pain going up and down the stairs, it can be pain with getting out of a chair, or getting in and out of the car.
“Studies have shown that people who have osteoarthritis have higher levels of depression, compared to people who don’t.”
“These are everyday activities that we take for granted,” she says. Eventually, the pain can reach a point whereby it impacts our ability to do sports, or even our ability to go to work.
“The other thing it can have an effect on is our mood,” says Dr French. “The studies have shown that people who have osteoarthritis have higher levels of depression, compared to people who don’t. And that kind of makes sense,” she adds. “If people have pain, they can’t do their everyday activities, they can’t do everyday movements – then they start to get depressed.
“That’s another thing we need to recognize can be a problem.”
Who is at risk?
Gender, lifestyle habits, age, genetics and weight all impact upon our likelihood of developing the illness.
For example, osteoarthritis affects women twice as much as men. “One in five women is at risk of getting arthritis,” says Dr French. Not only that, but the disease can impact people of any age. “While it is associated with getting older, young people can actually get arthritis as well,” she says.
“We often think of it affecting people in their 70s and 80s. But actually, it can affect people even from the age of 45 or 50.”
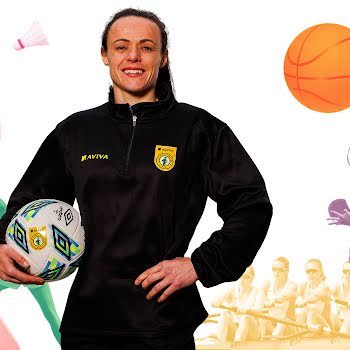
Sportspeople who’ve had a knee injury (such as an anterior cruciate ligament, or ACL) are also at high-risk. “In fact, women are more vulnerable to getting an ACL injury than men. You could have a girl in her 20s playing some kind of sports (like soccer or basketball) – a twisting-turning sport – and they can injure their ACL. So when they get into their 30s, just 10 years later, they could develop osteoarthritis.”
Apart from a joint injury, the biggest risk factor is obesity. “The more weight going through a joint, the greater the risk of developing arthritis,” says Dr French. “For example, for every five kilograms of weight, you’re increasing your risk of knee osteoarthritis by 36%. That’s quite a substantial risk,” she says, adding, “The risk increases threefold with people who are above the accepted weight limits.”
Preventative actions
Adapting to a healthy, active lifestyle is the best way to try and prevent osteoarthritis. “Being active, preventing injury as far as possible, and then keeping a good weight are three things I would be trying to get across. We don’t want to wait until people hit their 50s and start worrying about getting arthritis,” Dr French says. “Prevention is better.
“Maintaining a healthy weight (even as a young adolescent and into adulthood) is important. There’s lots of research to show that if you’re overweight in adolescence or as a child, you’re more likely to stay overweight into adulthood.”
What’s more, “if people don’t exercise as young adults, they are less likely to exercise as they get older.”
“There are lots of things to try before surgery.”
Unfortunately, arthritis is on the increase in Ireland for two main reasons. Not only are we are getting more obese (“Ireland has really high levels of obesity compared to other countries”), but we’re also living longer. “Arthritis is going to become more common over the next decade,” Dr French says.
“We’ve had lots of studies from lots of countries; we’ve had lots of guidelines, from research associations, from government organizations, from professional associations; and they’re all saying the same thing. In terms of managing osteoarthritis, the first line of management is exercise, education (people need to understand what arthritis is) and weight management.”
Things like medications and surgery are the next options. First, it’s about how people can take control of arthritis themselves. “There are lots of things to try before surgery.”
Nothing will change overnight
The difficulty in reducing osteoarthritis lies in our reluctance to change our behaviour. We are creatures of habit, after all.
“The problem is when we ask people to exercise more, to lose weight, it’s like people going on a diet,” explains Dr French. “People can do these things for short periods of time, but it’s the long term adherence is the real challenge. How do we get people to adhere long-term to these lifestyle behaviours that can both prevent and manage arthritis? It’s the long term solutions we need to address.
“And also, the health systems we have in Ireland currently may not be optimal for helping people. As well as people looking at an individual level (at what they can do themselves), we do need to improve our health system,” she says.
“We have to look at it at different levels – at a personal level, and at a systems level.”
Quality of life
While osteoarthritis can be painful and impactful on life in many ways – it can also be well-managed, with many people going on to live normal, healthy lives.
“The progression of arthritis is quite variable. A lot of people think it’s definitely going to get worse, but research has shown (and even patients I have seen), will actually stay fairly static and not get worse. Some people can actually get better if they can maintain good weight and good exercise habits,” she says.
“People can resolve their symptoms. We can’t repair the cartilage, because it needs good blood supply, but we can certainly try to manage the symptoms – which is the pain and people’s ability to move and function.
“That’s what we focus on. We focus on trying to improve people’s ability to move. And if you can move better, that has a knock-on effect on work, enjoying life and being able to get out and do things.”
If you are experiencing any symptoms of arthritis, contact your GP or local healthcare professional.
Dr Helen French is a senior lecturer in the RCSI School of Physiotherapy and clinical specialist physiotherapist. For more information, visit rcsi.com.