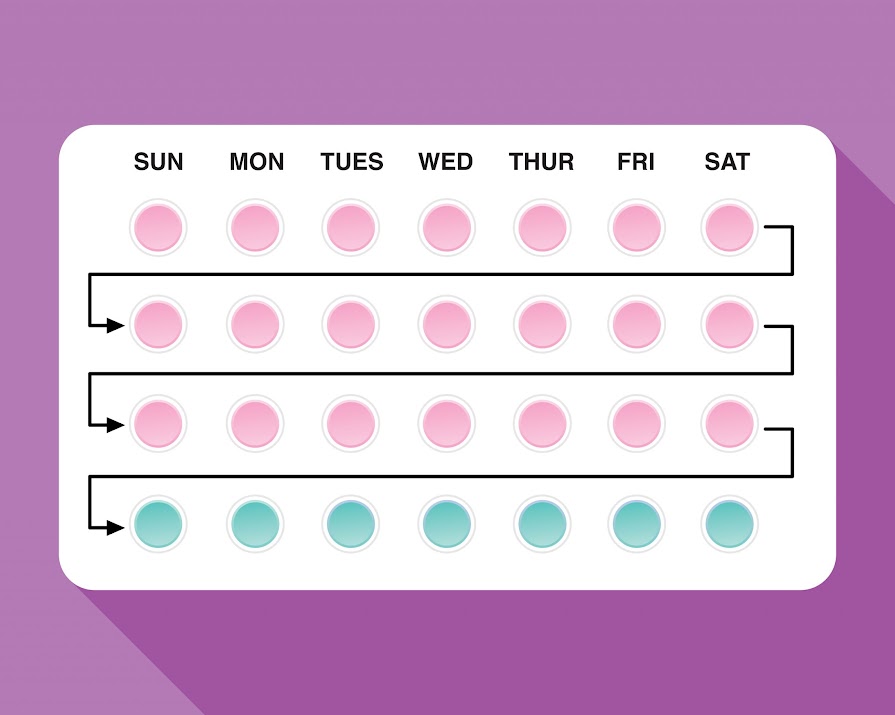
If we’re talking about blood clots, we should be talking about the Contraceptive Pill
By Jennifer McShane
13th Apr 2021
13th Apr 2021
Research indicates that the risk of blood clots is higher if you are on the pill, pregnant or six weeks post-natal than it is if you get the AstraZeneca jab. But while use of the vaccine is being reduced, almost no one is talking about making the pill safer for women.
The context: Last night, Ireland’s National Immunisation Advisory Committee advised that the AstraZeneca vaccine should be used only for the over-60s, as investigations continue into cases of blood clots in younger people. It follows from last week when the Joint Committee on Vaccination and Immunisation (JCVI) issued a statement about “extremely rare” cases of blood clots combined with low platelet counts in a small number of people who had the Oxford-AstraZeneca vaccine. No such cases have been reported in recipients of the Pfizer-BioNTech or Moderna vaccines.
The JCVI experts emphasised that the benefits of the protection that the AstraZeneca vaccine offers against Covid “far outweigh” the risks of an adverse reaction in the vast majority of people. But the committee is advising that adults under 30 without underlying health conditions should be offered an alternative vaccine “if available”.
Drugs regulator Medicines and Healthcare products Regulatory Agency (MHRA) found by the end of March, 79 people in the UK had suffered rare blood clots after vaccination – 19 of whom had died. The MHRA added that they estimate that the overall risk of these blood clots is approximately four people in a million, or one in 250,000, who receive the vaccine. A report from the BMJ, equates to about the same odds of “being hit in your home by a crashing aeroplane”.
Contraceptive Pill: A”higher risk” of blood clots
Another report on Sky News pointed out that the US National Blood Clot Alliance estimates that one in 1,000 women who are taking birth control pills will develop a clot each year. And the chances of developing deep vein thrombosis on a plane journey of more than four hours is around one in 4,656 flights – much higher than the risk for those who get the Oxford/AstraZeneca jab.
So why isn’t this being actively brought into the conversation more?
Research published in The Lancet found that oral contraceptives tripled the risk of blood clots, a risk which only further increased with obesity and a family history of blood clots.
According to UN figures from 2019, 842 million people use hormonal contraceptives. When it comes to hormonal methods of birth control, especially those that use estrogen, the person taking these pills is at a higher risk of blood clots.
Yet we’re hearing nothing from leading health organisations, as they scramble to adapt, alter and create new COVID vaccines, of how they could use this opportunity to re-examine a key component of women’s healthcare; experts (usually male) simply spout the numbers and urge the public to continue getting jabbed.
This sadly is not an unusual situation; when it comes to healthcare for women, we’re frequently left on the backburner. The CervicalCheck scandal in Ireland is a prime example of this. Women and their families (including women who died from this negligence) were compensated but rarely was liability admitted or an apology given. Accept it and move on is what this equates to – only families lost their wives, mothers, friends, sisters as a result will never accept it nor be able to fully move on.
“If men got pregnant, please believe that the contraceptive pill would have NO side effects,” wrote comedian Grace Campbell on Instagram. And you know what?
She’s right.
“Remember when the trial for the male pill stopped because men got mood swings?!”
So, maybe when we’re talking of life-altering side effects, we could look at a pill women must take every day for varying reasons when it comes to their health and wellbeing (knowingly putting themselves at risk) and how it could be changed for the better.